Rhythmology is a cardiology specialty dedicated to treating cardiac rhythm abnormalities, extrasystoles, uncontrolled heart rate (atrial fibrillation, atrial flutter, junctional tachycardia, etc.) or abnormal slowing of the heart (sinus mode dysfunction, atrial-ventricular block).
The goal of this consultation is to determine whether the perceived or observed problems are physiological or abnormal, to determine whether additional exploration is needed and to identify the most appropriate treatment, whether medication-based or interventional. The consultation also provides an opportunity to evaluate the inherited risk of certain hereditary rhythm problems, sometimes by performing a genetic survey.
In addition to the simple resting electrocardiogram (ECG), a stress ECG or a long-term ECG recording, whether using a continuous monitor (Holter monitor for 24 to 72 hours) or an event monitor (occasional recordings of heart rhythm abnormalities, for 1 to 3 weeks) may also be suggested.
Interventional rhythmology includes explorations and interventions that analyze or treat a rhythm problem or, in some cases, cardiac insufficiency. Most of these procedures are carried out under local anesthesia, sometimes with sedation, and more rarely under general anesthesia. Depending on the case, they can be performed on an inpatient or outpatient basis. Information sheets for each procedure have been created by the French Society for Cardiology (Société Française de Cardiologie) and can be downloaded at http://sfcardio.fr/fiches-de-consentement-patient.
External electric shock:
delivered under brief general anesthesia, to try to reestablish a normal heart rhythm in the event of uncontrolled atrial activity (atrial flutter or fibrillation)
Internal electrophysiological exploration:
exam enabling study of the state of the heart’s electric circuit, and to identify abnormal rhythms and their cause.
Implantation of subcutaneous ECG recorders:
Able to function autonomously for approximately 3 years, these recorders continuously monitor the heart rhythm and can record occasional anomalies (uncontrolled activity, slowing, palpitations). In some cases these recorders can be monitored remotely via “telecardiology”.
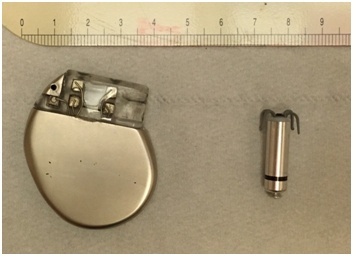
Implantation of cardiac pacemakers
for treating abnormal slowing of the heart beat, which could cause syncopes. Depending on the patient’s needs, devices can be implanted that are connected to the heart by one lead (single-chamber stimulator), two leads (double-chamber stimulator) or three leads (triple-chamber stimulator or resynchronizer, used to treat certain forms of cardiac insufficiency). Leadless pacemakers are miniature cardiac pacemakers without any leads that are implanted directly into a single ventricular chamber after being passed through a vein in the groin crease. In some cases these devices can be monitored remotely by “telecardiology”.
Implantation of cardiac defibrillators,
which are used to treat serious uncontrolled heart rhythms in at-risk patients (history of ventricular tachycardia or ventricular fibrillation; altered heart ejection fraction). As with all stimulators, depending on the case, a single-, double- or triple-chamber defibrillator is implanted. For patients requiring a single-chamber defibrillator, instead of using a conventional defibrillator, a subcutaneous defibrillator without an intracardiac lead can be implanted. In some cases these devices can be monitored remotely by telecardiology. For indications that may only potentially require a defibrillator, a wearable defibrillator vest may be prescribed for a limited period of time.
Removal
of leads, stimulators or heart defibrillators.
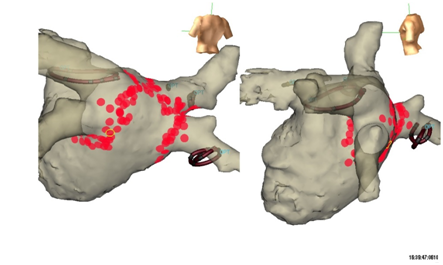
Ablation of cardiac arrhythmias:
a number of cardiac arrhythmias can be treated and often healed by ablation (flutter, atrial fibrillation, junctional tachycardia, some common ventricular extrasystoles, etc.). These interventions involve destroying the area of heart tissue causing a patient’s arrhythmia using heat (radiofrequency current) or cold (cryoablation). Some complex ablations require three dimensional mapping systems to treat them as effectively as possible.
Implantation of left atrial appendage occlusion devices,
used for some patients who are at risk of developing blood clot embolisms at the exit of the heart, when anticoagulants cannot be used.