Epidemiology
Kidney cancer represents 3% of all adult cancers, with a male/female ratio of approximately 2/1. Its frequency increases with age until 65: one out of two cancers is diagnosed before the age of 65. In 2012, 11,500 new cases were reported, and 13,000 in 2015. Due to ultrasound and CT scan assessment, this cancer is discovered earlier, which means it is often treatable by partial surgery, meaning only the tumor is removed.
Risk factors
Tobacco use, significant obesity, high blood pressure and renal insufficiency in patients on dialysis. There are family forms represented by rare genetic diseases. Some professional exposures: petrol products and heavy metals.
Treatment
Surgical. The details of the procedure are discussed in Multidisciplinary Team Meeting (MTM) attended by the entire urological team from the Ambroise Paré Clinic (seven urologists), radiologist, oncologists and anatamopathologists.
Surgeries
Partial nephrectomy
Only the tumor is removed; the rest of the healthy kidney is left intact to preserve as much of your renal function as possible.
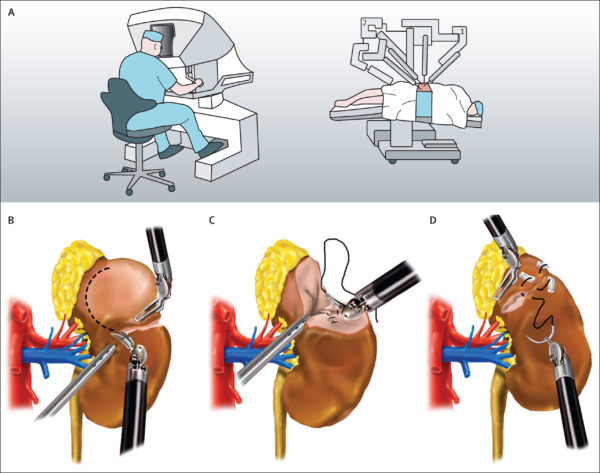
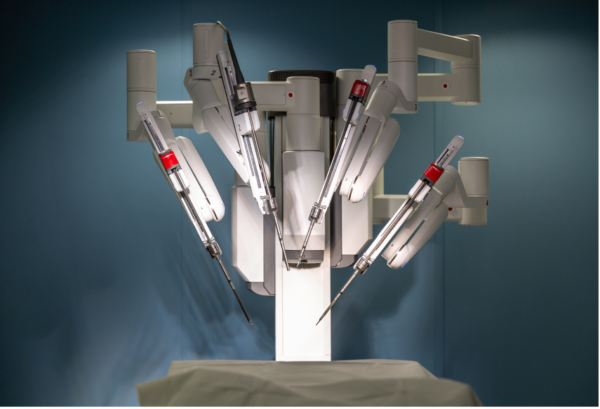
Using the Da Vinci surgical system: this is the technique that we have used in the majority of cases at the Ambroise Paré Clinic for more than 10 years.
We have a latest generation Da Vinci robotic surgery system. This is a particularly powerful tool that enables us to perform surgeries that are as precise and conservative as possible. The three-dimensionality, high-resolution visibility, instrument manipulability and related technologies (intraoperative ultrasound, Firefly technique, etc.) allow conservative interventions to be performed in a very large number of cases, including lesions up to 7 cm.
 Néphrectomie
Néphrectomie
Partial nephrectomy: DA VINCI ROBOT
Digitally enhanced precision
-amplifies gestures
-eliminates fatigue tremors
The surgical procedure consists of removing the tumor while preserving the healthy kidney. In most cases, the blood supply to the kidney must be temporarily interrupted using clamps (temporary blockage of the blood vessels that supply the kidney) for the time it takes to remove the tumor, after which the kidney is sutured. All of these steps can be performed more precisely and more quickly due to robotic technology, which limits the duration of kidney ischemia and limits blood loss. The tissue removed during the procedure is then subjected to microscopic analysis as part of the anatamopathological exam.
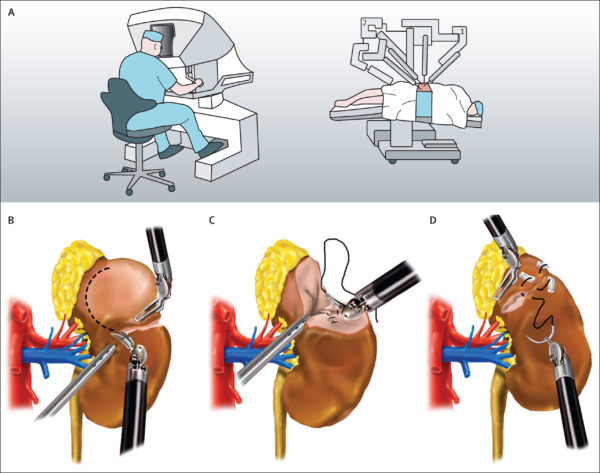
As the scars (generally 5 or 6) are small (1 cm), post-operative recovery is faster, particularly as the trauma to the muscle wall is substantially reduced compared to conventional open surgery.*
Total nephrectomy
The entirety of the diseased kidney is removed. This intervention is most often performed by robot-assisted laparoscopy, and in rare cases as an open procedure. Once the date of the surgery has been determined by your surgeon, he or she will provide you with a file containing information about your stay, how the procedure will be performed, the different tests that will need to be performed, contact information for making an appointment with the anesthetist and the details of the admission procedure.
*open surgery: this means making a traditional opening called a lumbotomy incision.
Preparing for the procedure
An anesthesia consultation must take place at least one week before the intervention.
Inpatient stay
You will generally be required to stay at the hospital for 5 days, in a shared or private room depending on your preference. You will be welcomed to the urology service on the 6th floor the day before your procedure by our administrative assistant ELSIE (Tel: 01 46 41 87 75) and by the floor’s medical and paramedical team. This team will collect your medical file, and particularly your radiological file. The day of the procedure you will be taken down to the operating room and then put to sleep, as the intervention is performed under general anesthesia. The length of the procedure varies, depending on your case. Once the procedure has been completed, you will be transferred to the recovery room where a specialized team will take care of you before authorizing your return to your room. You will not be able to have your first meal until the following day.
Care at the Ambroise Paré Clinic
Care will be provided by a nursing team and nursing assistants who specialize in urology, as well as by physical therapists. The anesthetist and the surgeon will see you every day until you are discharged.
Discharge
Elsie will give you your prescriptions when you leave (at-home nursing care, any medications needed, biological exams to be performed) and will let you know when your next appointment is.
Recovery
You will be allowed to resume as normal a life as possible (walking, using stairs, although you should avoid lifting heavy objects for a month) in the place of your choosing. While it is recommended that you not drive for the first 10 days following discharge, you can be a passenger. You can resume your normal eating habits.
Medical follow-up
The first post-operative appointment will take place one month after you leave the clinic, after which your surgeon will determine the frequency of subsequent follow-up visits.
 Néphrectomie
Néphrectomie